Researchers at Brigham and Women’s Hospital in Boston have identified the driving force behind severe inflammation in asthma. Results from their study, “Mast Cells Control Lung Type 2 Inflammation via Prostaglandin E2-Driven Soluble ST2,” were published in Immunity.
Prostaglandin E2 (PGE2) is a chemical in the human body previously thought to inhibit mast cell activation. Instead, it elicits mast cells, inhibiting inflammation by creating the molecule soluble ST2 (sST2). This molecule mitigates signs and symptoms of asthma by blocking the actions of interleukin (IL)-33. The research supports the notion that mast cells don’t merely drive inflammation, they serve a dual role in mitigating it when PGE2 is present. PGE2 is known to suppress the inflammation associated with asthma exacerbations.
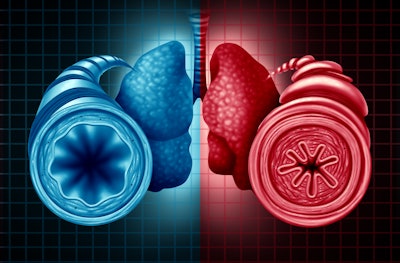
“Severe asthma and sinus disease are consequences of type 2 inflammation (T2I), mediated by IL-33 signaling through its membrane-bound receptor, ST2,” the researchers wrote. “Soluble (s)ST2 reduces available IL-33 and limits T2I, but little is known about its regulation. We demonstrate that prostaglandin E2 (PGE2) drives production of sST2 to limit features of lung T2I.”
The study, which involved mouse models with airway inflammation, explored inflammation severity from the impact of deficiencies in PGE2, the loss of PGE2 receptors from mast cells and the absence of ST2 from mast cells. Researchers also noted that levels of PGE2 metabolites in urine were associated with serum sST2 levels in patients with severe asthma and nasal polyps. High serum sST2 levels were associated with less severe disease and improved lung function.
“Mast cells likely protect against the mechanisms that drive severe inflammation under conditions of normal PGE2 generation,” researchers said. “However, when PGE2 isn’t produced sufficiently, which is common in severe asthma and nasal polyposis, the lack of mast cell-derived sST2 contributes to the severity of disease. Our findings suggest a promise in targeting PGE2 with therapeutics to alter the levels of sST2 in patients with severe asthma. They also suggest that antibodies against ST2 and IL-33, currently in clinical trials, may work best in patients with the lowest levels of PGE2 production.”
Moving forward, researchers will look at the possibility that PGE2 and sST2 levels can impact the success of new drugs, including monoclonal antibodies, which are developed for the treatment of severe asthma and nasal polyposis.























